If you’re looking for low cost health insurance in New York and have a pre-existing condition, the amount you pay for health insurance may seem low, but you will be making up for it in out-of-pocket expenses. Why? Because your new health insurance company might not pay for the cost of treatment for the pre-existing condition right away, which means you’ll have to pay for treatment yourself.
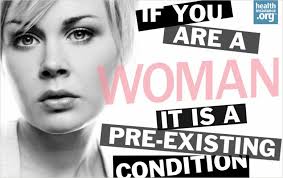
What exactly is a pre-existing condition?
Health insurance companies consider pre-existing conditions to be any health conditions for which you have been treated during the six months prior to applying for low cost health insurance benefits. During those six months, if your doctor or other health care professional recommended treatment for a condition, that condition is also considered a pre-existing condition regardless of whether or not you actually obtained treatment for the condition.
How does a pre-existing condition affect my health insurance benefits?
It doesn’t really affect your benefits, per se, but it does affect what is covered and what isn’t.
If you’re applying for new low cost health insurance in New York and have a pre-existing condition, it’s very possible that you will have to wait for 12 months before your pre-existing condition will be covered under the low cost health insurance policy. This means that the health insurance plan won’t cover the costs of any treatments from any doctors or other health care professionals during those 12 months.
Do I have to wait the entire 12 months?
The time you must spend waiting for the costs of your pre-existing condition to be covered by your low cost health insurance plan in New York could be shortened, though. If you went no longer than 63 days without health insurance benefits during the last time you had health insurance benefits, the low cost health insurance company will have to deduct the amount of time you had continuous coverage from your 12-month waiting period.
• What is a pre-existing condition and can it be excluded from my health coverage?
• Ans: A pre-existing condition is any condition for which a person received treatment or treatment was recommended within the preceding six months.
Any individual enrolling in a new health plan covered by NYS law may be subject to up to a 12 month waiting period (six months for Medicare Supplement policy holders) before expenses related to the pre-existing condition are covered. However, the plan must subtract from the waiting period the time that the person had continuous coverage in a previous plan. Continuous coverage means that the person had less than a sixty three day gap between each coverage. The insurer shall count a period of creditable coverage for all benefits or may elect to credit coverage based on Categories of Benefits specified in the policy or certificate.

0 comments :
Post a Comment